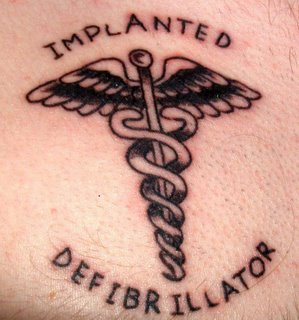
 Here's Dave's brand new tattoo. After some scheduling glitches, he finally got to the tattoo studio on the day before Thanksgiving.
Here's Dave's brand new tattoo. After some scheduling glitches, he finally got to the tattoo studio on the day before Thanksgiving.
Brugada Syndrome is a serious medical condition that causes sudden cardiac death in apparently healthy individuals. Sudden death is caused by severe disturbances in the rhythm of the heart. In this blog, you'll learn more about Brugada Syndrome, including what should be done if someone you know might be at risk of having this syndrome. You will also learn how I came to know so much about a condition that most people, and some doctors, don't recognize.
Sunday, December 11, 2005
Monday, October 17, 2005
He's going to get a tattoo next weekend.
I'm glad I didn't come of age in a time when tattoos were a "rite of passage". Perfectly normal young people who would consider tattoos to be an unacceptable insult to their bodies become enamored with the idea right around their 18th birthday. What a coincidence: when you turn 18 in New York State, you can legally go get yourself a tattoo. And many do.
Of course I "googled" the relative safety of getting a tattoo if you happen to have an implanted defibrillator in your chest. The results were mixed. Apparently some of the equipment used in the process of applying the paint contain magnets but pose no greater danger than, say, your cell phone. Keep it 6 inches from your ICD and you'll be fine, they say. Others seem to think that the wise thing to do is to skip it. But that information was probably written by an OLD PERSON. (You know, over 50.)
I'll post a photo of Dave's tattoo here next week. Dave, send me a photo, will you?
Sunday, October 02, 2005
At the end of the interview, the moderator asked Dr. Brugada what advice he offers the average person regarding Brugada Syndrome, and Dr. Brugada said that if a young healthy person dies in your family and the cause of death is not apparent, the family should see their doctor to investigate whether or not they might have Brugada Syndrome, but otherwise, this isn't the kind of thing that one should worry needlessly about.
I like Dr. Brugada and his reassuring approach to healthcare management for this condition. I also defer to his experience and knowledge on the topic. Perhaps concerns that I expressed in an earlier post may be unwarranted. Still, I know that when I hear of someone with unexplained spells of blacking out, or an episode of SIDS in the family, I always suggest that an ECG be reviewed to rule out Brugada Syndrome. But that's just me.
Monday, September 26, 2005
 Here is a lovely tee shirt that belongs to Dave.
Here is a lovely tee shirt that belongs to Dave.He purchased it through Medtronic Corporation, the manufacturer of his and Jim's ICDs.
Jim has his own Medtronic shirt. It's a real hoot whenever one of them has this shirt on!
While driving home from the store this evening, I heard Medtronic Corporation named as a sponsor of BBC World News heard on National Public Radio. Go Medtronic!!
Sunday, September 25, 2005

hand over heart! Very cute!
Do you know the difference between cardiac arrest (heart attack) and sudden cardiac death? They both sound pretty ominous! Well here is an explanation that a cardiologist offered to me: think of cardiac arrest as a problem with the plumbing. There is a clog or obstruction somewhere which is severely affecting the flow of blood to the heart. There can be varying levels of the problem. A person having a heart attack may experience several symptoms such as arm or jaw pain, nausea, stomach upset, chest pains. Heart attacks can cause minor damage to the heart muscle - or they can be fatal. It is imperative that a person in cardiac arrest receive medical intervention immediately. Long term treatment may involve heart bypass surgery, lifestyle changes, and medications such as blood thinners, beta blockers, and such.
In contrast, "sudden cardiac death" can be described as an electrical problem. There is a power failure, as though somebody just switches the power off. Period. There are no painful symptoms. Your heart stops beating properly, and within seconds, you lose consciousness. There is no treatment for Sudden Cardiac Death brought on by Brugada Syndrome. This is why patients are fitted with an implantable defibrillator.
We aren't sure exactly how common Brugada Syndrome exists in the population, one 2002 Italian study found "The current prevalence estimate is 1-5/10.000 in the Western countries. Higher frequency (1/2500) may be found in eastern countries, especially Thailand, where BrS is considered the major cause of sudden death in young individuals."
So in our small town, perhaps 5 to 10 people are walking around with Brugada Syndrome. And that is only one of several serious, diagnosable conditions that may lead to sudden cardiac death. There are others, such as Marfan Syndrome, or Long QT Syndrome. Should people be screened for these conditions, so that they may receive treatment?
In the United Kingdom, there is an active movement to raise awareness of sudden death syndrome and generally, cardiac risk of the young. One organization, C-R-Y, is working with the medical community to establish a national screening program. It recommends that youngsters receive a few screening electrocardiographs over the course of several years, with special attention to young athletes, a group at special risk for some cardiac conditions.
Electrocardiographs are noninvasive, quick and easy screening methods. But they aren't free. Is it worth the time and money to screen millions of people for such a rare condition?
The next time you read a sad story about a young healthy person who dies in her sleep, think about it: a routine screening electrocardiograph, conducted years earlier, just might have saved her life...
Saturday, September 24, 2005

Bill Clinton (former pres) and Roger Federer (current tennis star) both support the World Heart Association and announced World Heart Day through a joint press release. President Clinton had heart bypass surgery a year ago after experiencing chest pains. He maintains a healthy lifestyle, eats smart and stays fit. His Foundation is working hard to promote heart health.
Roger Federer, currently ranked the number one player of professional tennis, is the spokesperson for United Nations International Year of the Sport and Physical Education. You might have caught him beating Andre Agassi earlier this month. Wow was that a terrific match or what!! Anyway, he said, "Where ever you live in the world, moderate but regular exercise is extremely important. A small amount of exercise can make a big difference and help you have a healthy heart for life, too."
The World Heart Association is based in Geneva, Switzerland. Here in the U.S. , the American Heart Association, the American College of Cardiology, and the Children's Heartlink each have activities planned to promote awareness of heart health.
Sunday, September 18, 2005

So you have an ICD...Medic Alert tags - to wear or not to wear? - this is the question. (Here's a picture of Dave's.)
Only one problem. Dave won't wear his tag. He says it's uncomfortable. He worked as a line cook this past summer, and said that it really bothered his skin in all the heat. I think the tag is currently on his set of keys. So what good is it there?
I just don't understand tattoos.
Thursday, September 15, 2005
Dave's and Jim's surgeries were nearly a year ago, in October of 2004. Sometimes it seems as though years and years have passed since then. For lots of reasons.
I've added a link about Brugada Syndrome. It's from a different perspective - a website about genetic conditions, not cardiac conditions. Interesting reading.
Monday, September 05, 2005
Tuesday, August 16, 2005
 The Great Race
The Great RaceIn this photo is my son, Dave, in the center, with friends Mike (left) and Ben (right). Two days ago they participated in a popular annual run, bike and paddle race here in our town. They did a great job and had fun. Here they are recovering from the grueling canoe leg. They called their team "Dead Last" because they didn't do any serious training for the event, and expected to place last. But they didn't! Far from it. They were pleased.
The only time Dave's cardiac condition was an issue had to do with his defibrillator. It's recommended that ICDs be kept away from strong magnetic fields. This race uses a transponder system to accurately log times. This involves wearing a small disk, the size of a coin, that will be activated when the racer runs through a magnetic field. How strong is the field? Would it trigger Dave's ICD? He didn't know and so they simply made sure that the relay person was someone else on the team. Mike, not Dave. Mike met up with the biker, then ran to the canoe, and he and Dave were off.
Friday, August 12, 2005

Brugada Syndrome is more common that you might think.
Brugada Syndrome may be responsible for up to 50% of all sudden deaths that occur in individuals with apparently normal hearts. On the website maintained by the Brugada brothers who first identified the syndrome, they estimate that it may be indicated in somewhere between 4 and 12% of all sudden deaths.
A study of the ECGs of 12,000 non-cardiac patients in a large urban teaching hospital was undertaken to determine how many of them exhibited the classic Brugada Syndrome pattern. The results showed that 52 were found to have ECG patterns specifically consistent with Brugada Syndrome. The authors of this study note that Brugada Syndrome is much more prevalent than previously thought.
To put it into perspective, this means that in a high school with 2,000 students, you might expect that there are 7 students in that population who would test positive for Brugada Syndrome. Sobering information. In a future post, I'll discuss the status of routine ECG screenings of children in our country compared with other industrialized countries.
So if this is true, why haven’t we heard of it more often? Well, it is not a new disease, but it is newly diagnosed. Brugada Syndrome was first identified back in the early nineties by Drs. Josep and Pedro Brugada. It is hereditary, but having the syndrome doesn’t necessarily mean that the patient will be struck down by it. In my husband Jim’s case, he had no memory of anyone in his parents’ families dying young and healthy. It may skip a generation, or the affected relatives may have died of other causes before they might have suffered from a cardiac event brought on by Brugada Syndrome. Unfortunately, the statistics for long term survival of known Brugada patients are not great. The ICD is the only way to be absolutely sure a patient will survive sudden cardiac death.
In instances of young healthy children or adults dying with no explanation, or sudden crib death, or even episodes of fainting that can’t be explained otherwise, the survivors or patients should definitely be screened for Brugada Syndrome.
Because so many physicians in the United States have never encountered Brugada Syndrome, the onus may be on the patient to be diligent about follow-up if any of the circumstances I described above happen in your family. This is such a new syndrome, and the research is ongoing, that it’s possible for a very good physician to simply not be familiar with the disease.
(photo above is of my son Dave and daughter, Jessica, outside the White House lawn in 1990.)
Wednesday, August 10, 2005

How it all started…
The cardiologists told us that Dave was a healthy teenager, and his heart was strong and normal. They were at a loss to explain why it spontaneously developed an arrhythmia. But the digoxin, to help prevent further occurrences, and follow-up visits, reassured us and Dave went home and picked up life exactly where he’d left off three days earlier.
Six months later, during his follow-up visit, the doctor noticed a unique wave pattern in Dave’s ECG. We learned that day the Dave most likely had Brugada Syndrome. It's rare, and isn’t usually associated with cardiac arrhythmias or flutters. How fortunate we were, that Dave was under the care of cardiologists with the skill to notice this elusive condition. The gave us sobering news: if Dave did have Brugada Syndrome, he was at risk of experiencing sudden cardiac death at any time.
Brugada Syndrome is usually confirmed during an electrophysiology study (EP study) in which a catheter is threaded from a large vein in the groin to the heart. Here electrical activity can be studied and any arrhythmias can be mapped. The ventricle (lower chamber) is then prodded into fibrillation in a controlled setting. A healthy heart will not go into fibrillation. Another method that can be employed is to introduce certain drugs to stimulate fibrillation.
Dave went through the EP study, which confirmed his diagnosis. Before we had begun to absorb what was happening, he was scheduled for next day surgery to have an ICD (implantable cardioverter defibrillator) installed. This seems like a drastic step to take because the surgery is invasive and the ICD is costly. But we learned that there is no cure for Brugada Syndrome. The ICD will shock Dave’s heart back into sinus rythym if he has a Brugada event. Since Dave was at risk of sudden cardiac death, the choice here was simple. His ICD is the only assurance we have that Dave will survive such an event. At the top of this post is a picture of Dave taking a photo of his incision site the day he returned home from the hospital with his ICD.
The story doesn’t end here. Brugada Syndrome is hereditary. Our whole family was tested, and blood drawn for genetic study. My daughter and I showed no characteristic waves in our ECG strips, but Dave’s father, Jim, was found to have the syndrome. He, too, endured the EP study, and the subsequent surgery to have an ICD implanted. During the EP study was able to have an existing atrial arrhythmia condition treated successfully through a procedure called cardiac ablation, and this was good.
The doctor told my daughter that because her genetic make-up is identical to her brother's, she should have a new ECG strip run every now and then and sent to him for review just in case. Another confounding element of Brugada Syndrome is that is doesn't present in an ECG every time, it may appear and disappear over a person's lifetime.
Sunday, August 07, 2005
Brugada Syndrome is a serious medical condition that causes sudden cardiac death in apparently healthy individuals. Sudden death is caused by severe disturbances in the rhythm of the heart.
Here you will learn more about Brugada Syndrome, including what should be done if someone you know might be at risk of having this syndrome. You will also learn my family's story and how we came to know so much about a condition that most people, and some doctors, don't recognize.